A Chief Executive Officer (CEO) of a health system was determined to address workforce wellbeing. A physician himself, the CEO assembled a wellness committee, used conventional engagement tools, and asked the senior vice presidents to all focus attention on improving the wellness of their physicians, nurses, advanced practice providers, and other clinical staff. The health system invested in appreciation-related marketing, rounding, and many other efforts—but the staff continued to suffer from high turnover and worsening morale.
The challenge came to a head when a physician on the wellness committee, nearly in tears, argued during a public forum that the leaders simply weren’t listening. Dumbfounded by this incongruence, the leaders sought help to better forge a new path forward.
For many healthcare organizations, reversing the damage of the pandemic on an already strained workforce continues to be a thorny challenge. While most workers are motivated to be in the profession out of a desire to help people, many are still recovering from the trauma they have endured on the front lines in recent years. Simultaneously, high turnover rates are creating ongoing churn, putting extra pressure on experienced staff who have chosen to stay, and leaving many dissatisfied with the time they can devote to high-quality patient care.
Compounding the staffing shortage are the recent step-function increase in labor costs for employees and painful premiums for travel nurses and agency staff. Many leaders have exhausted financial tactics for attracting, retaining, and engaging their workforce. Although some organizations have stabilized their staffing levels and reduced their dependence on travel nurses, elevated labor costs are likely to persist for all organizations. The labor market remains tight, and demographic trends show more individuals are retiring or otherwise leaving the field than replacements are being trained.
While each organization faces unique workforce challenges, it’s become apparent that “softer” workforce tactics like pizza parties, picnics, and service pins are not addressing root causes. In fact, a recent study of nurses found that such activities were actually “more likely to harm morale than help.”1 Meanwhile, the most common tool to guide interventions—engagement surveys—can provide a high-level sense of morale but may not provide granular insights to drive retention and recruitment.
Determining which changes will make the most difference and where to focus effort and resources is challenging. These 4 strategies can help leaders deploy the solutions and integrate the routines that will sustain their workforce and position their organization toward becoming an employer of choice:
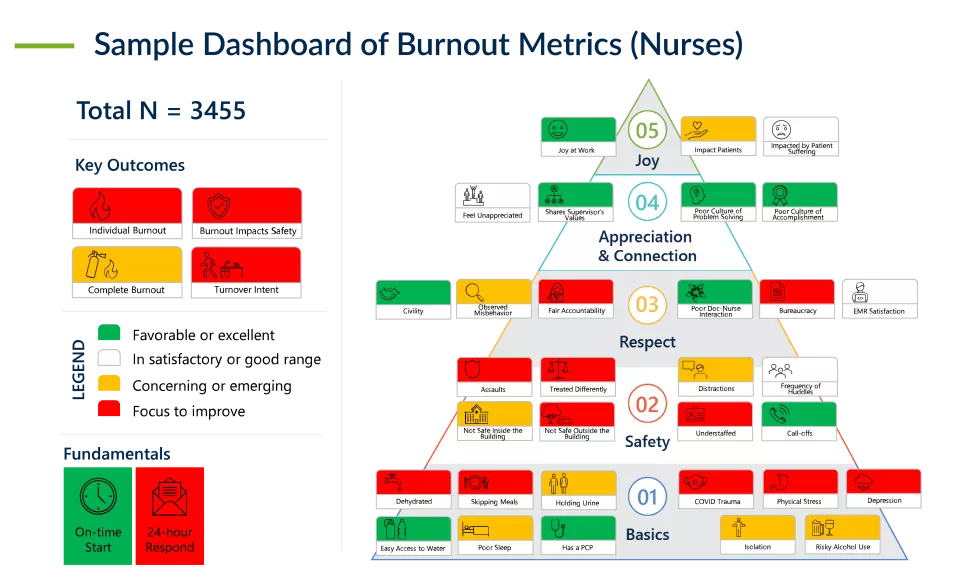
- Assess the key needs of the workforce: Identify detailed pain points and drivers of burnout—by department, unit, role, and other segmentations—because experiences differ within individual organizations.
- Improve the daily work experience: Enable teams to efficiently provide care and support at the top of their practice capabilities.
- Reinforce cultural connections: Ensure that the personal and professional commitments the organization makes to employees are visible, sustained, and comprehensive.
- Advance the supporting infrastructure: Promote leadership accountability with management systems that effectively attract and retain staff, build future workforce pipelines, and measure and monitor progress against workforce sustainability goals.
Taking a comprehensive, holistic approach requires a focus on ongoing two-way communication between senior leaders and front-line managers and staff, and alignment and financial investment to effectively execute a workforce transformation. While the work can be complex and the commitment significant, so is the expected return— increasing worker health and engagement, minimizing turnover, reducing dependence on travel nurses, improving patient experience, and becoming the regional employer of choice.

Sources: 1 U.S. Bureau of Labor Statistics; 2Saratoga, Industry: Hospitals and Health Systems; 3AMN Healthcare 2023 Survey of Nurses; 4“Trends in Clinician Burnout with Mitigating and Aggravating Factors during the Covid 19 Pandemic,” Linzer et al, JAMA Health Forum; 5Syntellis, All Hospital System Benchmark; 6ANA website
1. Assess the Key Needs of the Workforce, Especially the Drivers of Burnout
The first step is to carefully assess your workforce’s experience, with a special focus on the drivers of burnout. In addition to its immense personal toll, burnout is one of the greatest engines for turnover.2 It is predictive of worsened safety and quality, higher incidence of malpractice claims, poorer patient satisfaction, and reduced productivity.3 And it can breed cynicism and erode morale.
In our experience, annual staff engagement surveys are helpful to take the average temperature of the workforce. Yet to uncover the specific nuances and extent of daily challenges individuals face, a more detailed, focused approach is often required. Not only is each institution unique, so is each employee’s daily experience and drivers of dissatisfaction and burnout. These can vary widely by role, specialty, department, unit, age, length of service, and gender.
Demographics and “local details” matter. Solutions will only be successful if tailored to the distinctive attributes of the organization’s operations and culture. Consequently, it’s critical to regularly harvest insights to identify targeted improvements and monitor progress.
A multi-faceted, comprehensive approach will provide an accurate current-state assessment. This approach should include:
-
Interviews with organizational leaders, operational managers, and other key stakeholders, such as select leaders across clinical, administrative, and support areas.
-
Detailed surveys and focus groups tailored to different occupations, roles, and levels of seniority.
-
Targeted analytics (e.g., gaps in staffing, turnover rates, and recruitment yield) and comparisons to leading practices to identify areas for prioritization.
-
In-person observations in nursing units and other high-opportunity areas.
Quantitative and qualitative data should be synthesized in a way that is easy to interpret and can inform the development and prioritization of solutions. A sample dashboard of metrics related to burnout is shown below.
Example
A Targeted Solution Is Built Around Local Staff Experience
A CEO of an academic health system faced high burnout and turnover intention among internists and specialists. After an assessment, she was surprised to learn that many physicians felt tortured by the wide-open patient portal and its cluttered, difficult interface. About one-third of these physicians had strong screeners for their portal messages, but the other two-thirds had little help and felt they were spending extensive time on uncompensated efforts well below their licensure level. She prioritized reducing the time spent in the portal and invested in IT assistance to drive down the hours physicians spent screening messages themselves.
2. Improve the Daily Workforce Experience, Starting with Assessment Results
While organizations may deploy a range of solutions to address both common pain points across the organization and unique friction points experienced in specific roles or departments, these efforts should be coordinated and comprise a holistic approach to improving workforce wellness.
At the most foundational level, organizations must ensure basic human needs are met, such as ensuring consistent and adequate times for meal breaks so staff aren’t hungry or dehydrated, and a process for coverage during bio breaks.
In addition, organizations should offer a physically and psychologically safe environment. To ensure a physically safe environment, protocols should be reviewed and adjusted to protect staff from a range of physical threats, from bullying to gun violence. A psychologically safe environment involves building a culture of belonging, inclusivity, and respect, with no tolerance for behaviors or actions that deviate from those values. It also means establishing a timely, non-punitive process for responding to staff concerns or complaints.
Below are examples of other areas of opportunity organizations might prioritize based on their assessment results:
Assessment Finding |
Example Solution |
|
Key nursing and other staff positions are remaining open too long; the recruitment, hiring, and onboarding processes are too slow to keep up with current turnover. |
Develop a multi-year roadmap for critical positions to anticipate needs sooner; streamline talent acquisition processes from recruiting through onboarding to avoid losing great candidates; update written and oral messaging to candidates to better reflect their needs. |
|
Anticipated and unexpected gaps in nursing (e.g., for maternity leaves and personal medical leaves) leave units understaffed and remaining nurses overburdened. |
Create a “float pool” of nurses who have been trained in multiple types of units and who can flex in and out of those units as needed; cross-train and leverage support roles, such as tech or aide deployment, administrative, and support services generalist. |
|
Operational and clinical processes do not consistently enable optimal delivery of high-quality care that also offers a satisfying patient and clinician experience. |
Adopt high reliability principles; redesign processes to fix throughput issues; and establish regular monitoring and measurement of key metrics. |
|
Many nurses find it difficult to achieve a reasonable work-life balance with the current shift schedule. |
Offer a flex schedule option and/or coordinate the necessary support services to stand up a virtual nursing program in appropriate clinical areas. |
|
There is limited visibility into progress against key workforce goals; data and reporting are inconsistent across the organization. |
Establish consistent metrics and standardize workforce data (e.g., satisfaction, turnover, vacancy, productivity, engagement, and agency utilization) across sites and units; develop a standardized performance “scorecard”; and implement regular meetings to review the scorecard in each unit or at each site. |
|
Staff satisfaction is variable, with some units impacted much more than others. |
Develop targeted training programs that address specific behavioral and performance issues and cultivate best practices beyond patient care (for example, guidance for mid-level managers on how to have difficult conversations with colleagues). |
When prioritizing improvement initiatives, it is helpful to identify opportunities for “quick wins,” while also flagging areas that will likely require more in-depth planning, business case development, collaboration across leadership, and implementation timelines.
Additionally, organizations should evaluate their existing workforce-related initiatives to determine where current inflight workstreams need adjustment, sunsetting, or strengthening, and whether new approaches are necessary.
Example
A Coverage and Tracking Process to Ensure Meal and Hydration Breaks Produce Positive Results
A Chief Nursing Officer (CNO) recognized that dehydration is related to worsened cognition and mood. Frustrated with high rates of dehydration and skipped meals among her nurses despite hard work to make food and drink available, she implemented tracking of breaks and a coverage process that made them mandatory. Predictably, dehydration rates dropped precipitously and with them, a moderate but statistically significant reduction in burnout.
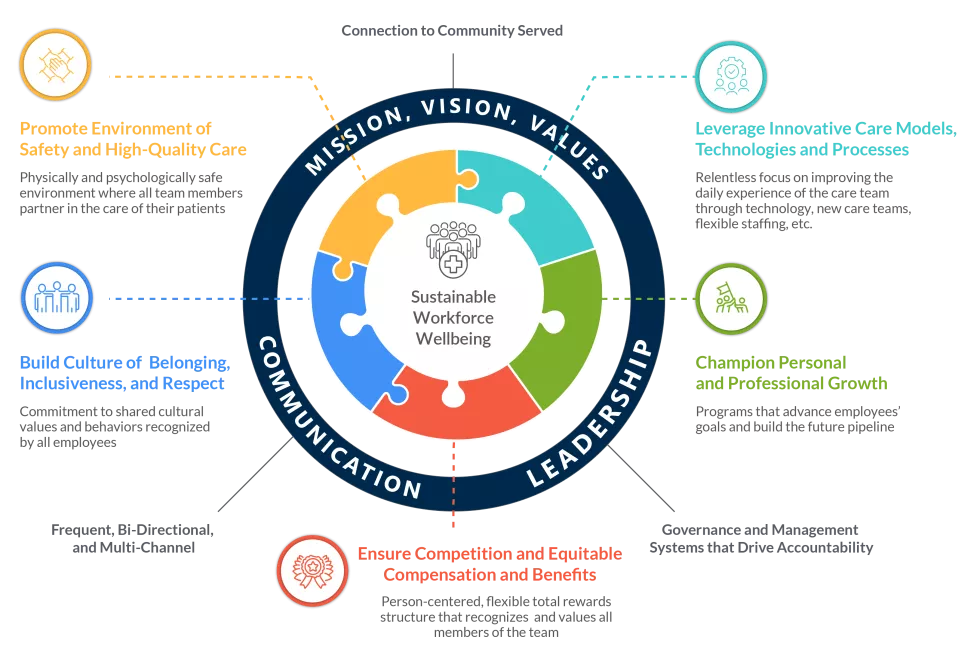
3. Reinforce Cultural Connections Between the Organization and Workforce
Most healthcare workers are strongly driven by the opportunity to serve and improve the lives of patients. Organizations that consistently communicate and amplify that mission, visibly demonstrating their commitment to the surrounding communities, are more likely to have engaged and dedicated employees.
First and foremost, the workforce should feel connected to the mission, vision, and values (MVV) of the organization, beginning with the recruitment and onboarding process and extending throughout an employee’s time at the organization. The MVV should reflect the voices of the people closest to the care that is provided and should foster a culture of inclusiveness, belonging, and respect. This requires active listening and responding to those voices, and embedding them within the MVV. The MVV should be lived out every day at all levels of the organization.

“Beyond Burnout Part II: What Nurses Want Now,” Jarrard, Inc., September 2023.

“Beyond Burnout: Trust, Loyalty, and the Physician Gender Gap,” Jarrard, Inc., June 2023.
Other examples that can strengthen the cultural connection between an organization and its workforce include:
- Restructuring the onboarding process to reduce paperwork and increase consistent personal connection.
- Addressing the social drivers of health for the organization’s lowest paid workers, including food insecurity and transportation needs.
- Providing in-the-moment assistance and visible escalation procedures to manage abusive patient behavior, including racist comments or violent actions.
- Establishing bi-directional feedback mechanisms with accountability for taking action.
- Offering a variety of support systems, which could include “opt-out” counseling for those with high levels of stress and/or PTSD, support groups, peer support systems, legal assistance, and/or financial assistance for those experiencing times of hardship.
Collectively, these efforts can build a culture of trust and improve the wellbeing of staff. A supported, healthy staff will be more able and motivated to deliver safe, high-quality care and more likely to feel a stronger connection to their organization, leading them to stay for many years.
Example
Nurse Manager Turnover Assessment and Improvement Initiatives Lead to Dramatically Improved Turnover Rates
A nurse leader struggled with higher turnover among her nurse managers than among her staff nurses for the first time in the decade she’d been in her position. Noting that many managers had recently ascended into roles with little training, she opted to “put the oxygen on the managers first,” starting with a careful assessment of turnover drivers that included accountability, span of control, and career growth. She addressed these drivers and added routine leadership meetings that included more playful work focused on expectations, gratitude, and managing daily tasks. Taken together, these initiatives dramatically improved turnover rates among managers, returning to pre-pandemic levels.
4. Advance a Robust Supporting Infrastructure for Optimized, Sustained Progress
As many organizations have learned, efforts to improve workforce wellness are not one-off projects but ongoing solutions. Sustaining improvements requires an organizational structure that optimally balances leadership and management resources across the institution, focusing on both strategic and operational needs. Management systems that effectively measure and monitor progress against workforce wellness goals, and that promote leadership accountability, are essential for long-term success.
In addition to staffing gaps and turnover rates, metrics should include the priorities identified in the initial assessment. Metrics might include productivity, reported burnout rates, recruitment relative to turnover, number of reported issues, and the percentage that were successfully addressed. Calibrated responses should be prepared for behaviors or processes that deviate from the intended best practice, and detailed plans should reorient toward the institution’s values and expectations.
The process for regularly reviewing the selected metrics should be paired with actionable steps that address areas where performance is lagging or where feedback has changed. Partnering operations leaders with front-line staff to work together can often move these key actions forward. Developing a cadence for messaging ongoing progress back to staff is critical for reinforcing trust and confidence in leadership over time. In our experience, it can also reduce cynicism even before observable improvement data is available.
Organizations also must consider how they will advance workforce infrastructure to support current and future workforce development. Mentoring and developing newly hired staff and leaders is a critical competency for organizations in this new era.4 Providing clinical education and support for existing staff, as well as facilitating educational partnerships with local and regional institutions to train the future workforce, will help ensure an adequate pipeline for future nursing, clinical, and technical support staff. This will require a comprehensive commitment to education as a key differentiator and may include subsidizing teaching positions and program development.
Taking a holistic approach to workforce wellbeing can have significant impact. Select results are illustrated below.

Learn how a health system recently took this holistic approach and dramatically reduced turnover, decreased burnout, and drove up employee satisfaction.
Help Your Workforce Flourish for Years to Come
The workforce crisis amplified by the pandemic wreaked havoc on many health systems and their ability to function. Health system leaders have expended enormous efforts trying to right the ship, and while some have seen improvements, others continue to experience high rates of burnout and turnover. Tactics employed in the past, such as financial incentives, have become standard across the industry and remain important yet no longer differentiate an organization or satisfy the complex, unmet needs of the workforce. A new, holistic approach is needed to move the needle and ensure enduring success.
By thoroughly assessing their staff, improving their daily work experience, reinforcing cultural connections, and advancing the infrastructure to support this work, health systems can turn the current reality on its head. Instead of contending with staffing gaps and high burnout rates, health systems can develop and support a thriving, sustainable workforce for the future.
Additional Contributors:
Alexandra Schumm, Principal and Vice President of Research, and Cynthia Bailey, Assistant Vice President of Consulting Operations
Sources
1. “Nurse Engagement Survey: It’s Time to Trust Your Gut and Ditch Old Habits,” Jarrard, Inc., October 2022, https://jarrardinc. com/jarrard-insights/special-report/2022/10/nurse-engagement-survey-its-time-to-trust-your-gut-and-ditch-old-habits/
2. Shasha Han et al, "Estimating the Attributable Cost of Physician Burnout in the United States," Annals of Internal Medicine, June 2019, https://pubmed.ncbi.nlm.nih.gov/31132791/
Brendan Martin, PhD, et al, "Examining the Impact of the COVID-19 Pandemic on Burnout and Stress Among U.S. Nurses," Journal on Nursing Regulation, April 2023, https://www.journalofnursingregulation.com/article/S2155-8256(23)00063-7/fulltext
Neeltje de Vries, RN, et al, "The Race to Retain Healthcare Workers: A Systematic Review on Factors that Impact Retention of Nurses and Physicians in Hospitals," Inquiry, December 2023, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10014988
3. Rikinkumar S. Patel, et al, "Factors Related to Physician Burnout and Its Consequences: A Review," Behavioral Sciences, November 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6262585/
4. In a recent survey of nurses, only 1 in 4 gave their institution high marks for the onboarding process, more than 1 in 3 said their institution did not give nurses early resources they need to succeed, and roughly 1 in 2 thinks that their institution is committed to the success and satisfaction of their experienced nurses. “Beyond Burnout Part II: What Nurses Want Now,” Jarrard, Inc., September 2023, https://jarrardinc.com/resources/national-nurse-survey-2023-request/